23 Dec 2020 Fertility Insurance Laws Defray Costs of Assisted Reproduction But Exclude Gay Men
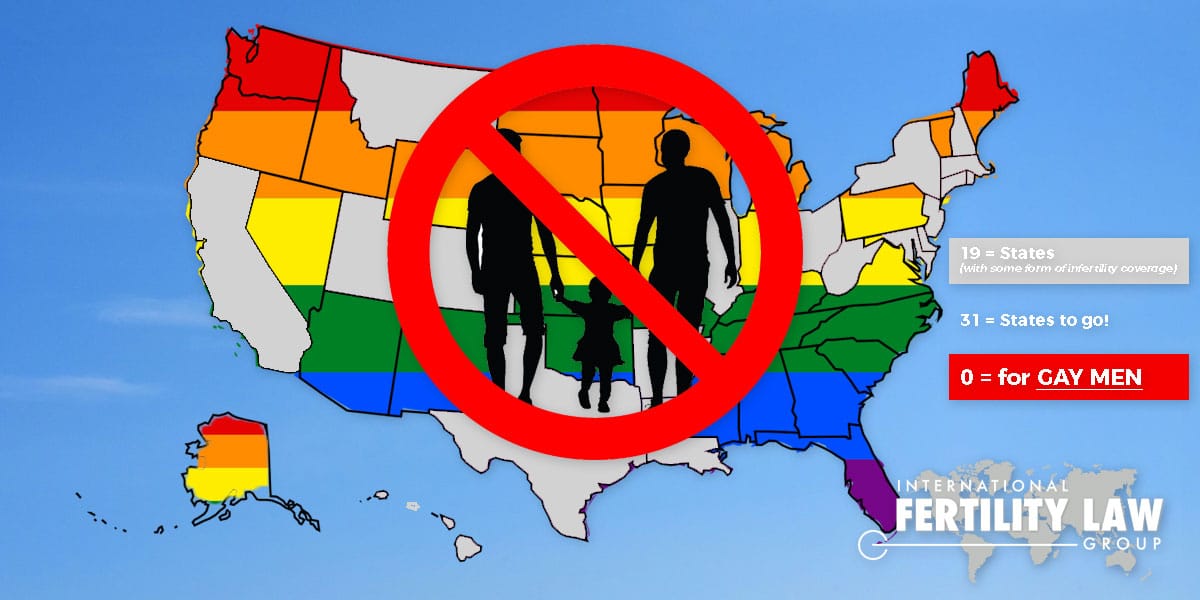
Nineteen U.S. states have enacted laws that require insurance companies to offer coverage for in vitro fertilization and other types of fertility treatments—a ray of hope for individuals for whom the high costs of assisted reproduction can be a barrier to parenthood.
But even as new laws prohibit discrimination based on gender or sexual orientation, insurers have found a “loophole” that allows them to deny fertility treatment coverage to men who are in a same-sex relationship—based on the law’s definition of “infertility.”
Now one couple has taken Blue Cross Blue Shield of Illinois to court, demanding the company provide them the same coverage for egg donation and IVF that it provides to single women and lesbians.
When Tee Lam and Adam Motz decided they wanted to become parents, they were fortunate to have loving friends ready and willing to help. Motz’s friend since high school agreed to be an egg donor; Lam’s longtime friend offered to be a surrogate.
All lights seemed to be green on Lam and Motz’s path to parenthood, until the couple submitted a $15,000 claim for costs of prescriptions for egg donation to their health insurance carrier, Blue Cross Blue Shield of Illinois (BCBSIL). To their surprise, their claim was denied, and an adjuster, in a recorded call, told Motz it was because they were two gay men planning to use a surrogate.
In the wake of coverage from NBC 5 Chicago, BCBSIL paid the couple $2,000, a payment Motz said was not related to their $15,000 prescription claim. The two are continuing to contest the claim denial.
BCBSIL said in a statement it is “committed to providing quality health care to members consistent with terms of their benefit coverage, regardless of sexual orientation.”
All Fertility Insurance Is Not Created Equal
The BCBSIL complaint highlights the reality that, even as more states require insurers to provide, or at least offer, coverage for fertility treatment, what is covered and who is eligible continues to vary from state to state and from employer to employer, as we wrote earlier.
According to RESOLVE, 19 states currently have some form of fertility insurance mandate, including 13 that cover IVF and 10 that cover fertility preservation due to iatrogenic infertility, or infertility caused by a medical treatment.
Many of the discrepancies in access and coverage hinge on the traditional definition of “infertility.” In Illinois, for example, the state’s Fertility Mandate requires that all group insurance policies covering more than 25 people that cover pregnancy also cover infertility diagnosis and treatment. But under the law, infertility is defined as “the inability to get pregnant after one year of unprotected sex or the inability to carry a pregnancy to term”—arguably criteria that would exclude gay men.
As part of their appeal to BCBSIL, Motz and Lam were required to submit a letter from Dr. Mary Wood Molo of Chicago’s Center for Reproductive health explaining why the two men were unable to conceive. Molo told NBC5 that although insurance policies typically cover costs for lesbians who undergo assisted reproduction, she did not know of any insurers who would provide coverage for a gay male couple. “For hetero and lesbian couples, yes, but not for same-sex male couples—with any insurance,” Wood Molo said.
After the U.S. Supreme Court legalized same-sex marriage in 2015, states began the slow process of changing laws governing reproduction and parentage to ensure they treated LGBTQ people the same as heterosexual people. In some conservative states, legislators have used gender-specific language within the laws to continue to discriminate.
And the insurance industry, which has always opposed laws that mandate specific types of coverage, appears to use legalistic definitions to deny coverage, even as it promises not to discriminate based on sexual orientation.
Even in Maryland, which has arguably the most inclusive fertility insurance mandate in the country, the language of the law still eliminates any possibility of fertility insurance coverage for gay males.
Prior to May 2015, Maryland law required that insurers provide treatment for fertility insurance only after a couple had a minimum two-year history of infertility, which insurers typically interpreted to mean two years of having intercourse without conceiving. Only fertility treatments using the husband’s sperm could be insured.
The new Maryland law specifically prohibits insurers that cover other types of fertility treatment from applying that restriction for same-sex couples. But the language of the law’s “Definition of Infertility/Patient Requirements” leaves no possibility the mandate for coverage could be applied to a gay male couple:
For a married patient, the patient and the patient’s spouse have a history of involuntary infertility, demonstrated by a history of:
- if the patient and the patient’s spouse are of opposite sexes, intercourse of at least 1 year’s duration failing to result in pregnancy; or
- if the patient and the patient’s spouse are of the same sex [emphasis ours], three attempts of artificial insemination over the course of 1 year failing to result in pregnancy…
It is the law’s one and only reference to same-sex couples, and it is clearly not applicable to gay men.
New York Fertility Insurance Law Relies on Outdated Definition of Infertility
New York is one of the most recent states to enact a fertility insurance mandate, expanding access to coverage to about 2.5 million people. But the new law continued to rely on an outdated definition of infertility, similar to Illinois’, to determine who is entitled to coverage. As we predicted in our earlier report, “Because of this definition, additional fine-tuning will be needed—either via legislation or court cases—to ensure that gay men or single men are not unfairly discriminated against.
Even more progressive states, such as California, which passed a law in 2013 clarifying that the fertility insurance coverage mandates should be applied equally regardless of sexual orientation, continue to rely on outdated and limiting definitions of infertility. In California law, infertility is defined as “the presence of a demonstrated condition recognized by a physician and surgeon as a cause of infertility or the inability to conceive… after a year or more of regular sexual relations without contraception.” Clearly, the definition was not intended to apply to gay males.
In contrast to the New York law, which requires a certain group of employers to provide coverage for infertility treatments, California requires only that insurers offer the insurance (which does not include IVF); employers decide whether or not to actually provide the coverage to their employees.
State by state, new laws requiring insurance coverage for infertility are making assisted reproductive services more affordable and accessible for more intended parents. But while lawmakers may intend to ensure coverage benefits all people regardless of sexual orientation, they continue to leave eligibility rules largely up to the health plans themselves. So even though states such as New York and California prohibit discrimination in offering coverage for infertility, the coverage itself is discriminatory because its definition of infertility eliminates gay men from eligibility. The result is injustice that will no doubt be remedied state by state, lawsuit by lawsuit, until state legislatures recognize that reproductive rights are human rights, regardless of gender or orientation.
I am quoted in this report by Dan Avery of NBC News, which has done a great job shedding light on Tee and Adam's story and the issue of insurance coverage for assisted reproduction.
For more information about becoming a parent through assisted reproduction technology and the legal issues involved, contact our experienced IFLG team of fertility lawyers and paralegals.

















